Endometriosis and THE WHAT? You mean to tell me that this disease can be found on your…spine? A disease typically diagnosed by gynecologists can grow there? Okay, now this is like some bad sci-fi horror film…But alas…it’s true. A girlfriend dropped the bomb last week that she has it on her spinal cord. So now it’s time to pick my jaw up off of the ground and hit the books. What the hell, Endo. Really? Is nothing sacred?
Spinal Endometriosis:
Endometriosis on or in the spinal cord, vertebrae, or nerves is considered extremely rare. However, it has been found to be wreaking havoc for many women. It can cause symptoms of back pain, weakness, incontinence, sciatica pain, radiating leg pain, groin pain, and monoparesis (weakness to the point of near-paralysis), just to name a few. These symptoms may always be present, may only be present during your menstrual cycle, or may worsen during your menstrual cycle. On top of those symptoms, the Endometriosis also does it’s usual thing: inflammation, scarring, creates pain, etc.
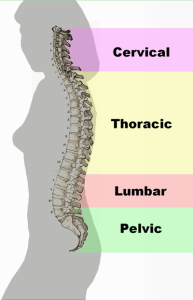
In seven different published case studies dating from 1968-2011, women ranging from age 26-46 complained of the aforementioned symptoms. Each was found to have Endometriosis inside or on the exterior of her spinal cord, nerves, or vertebrae; mostly in their lumbar spine, but one had it in her thoracic spine. Six of these women had surgeries to relieve the pressure in their vertebrae and nerves, as well as excise the implants and lesions. One woman did not have surgery, but underwent GnRH treatment. Six of those women stated that they were pain free after their procedures, and the seventh said she only had occasional pain after her surgery.
Diagnosis:
Your physician may be able to pre-diagnose spinal Endometriosis through an MRI and lab work; however, (just like we’re used to) the only way to truly confirm the presence of Endometriosis is through surgery.
Treatment:
Surgery : Endometriosis lesions and implants that are visible to the surgeon are excised or burnt off, and tissues are sent to the pathologist for testing and confirmation. Due to the sensitive and vital tissues of the spinal cord and nerves, complete excision of some Endometriosis may not be possible. A procedure to alleviate the pressure on nerves, vertebrae, or the spinal cord caused by the Endometriosis hemorrhaging may also be performed.
Birth control, hormone therapy, or GnRH treatments are also recommended to suppress symptoms of Endometriosis. Some women swear this has helped with their pain. Others, not so. As a last resort, (as usual…) we hear that a hysterectomy or oophorectomy (one or both ovaries are removed) may help with recurring Endometriosis symptoms, including the back and leg pain that may be associated with spinal Endometriosis. I personally believe that a hysterectomy is not a cure for Endometriosis. There have been numerous studies, time and time again, of women with recurring Endometriosis, sometimes decades after their hysterectomies.
Conclusion:
This is terrifying. Every site, study, or webpage I went to tonight in research pointed out that these pain and neurological symptoms should be taken very seriously. Have a talk with your doctor if you wish. Your spinal cord and nerves are very finicky and need to be well tended. As usual, this blog is not meant to scare you : only educate you. And I. And there are so many reasons why you may be suffering from back pain, including ovarian cysts as a cause.
Have you been diagnosed with spinal Endometriosis? Please, share your story. It’s a whole new world to me.
*Updated March 27, 2019*
Resources:
European Spine Journal (Abstract, May 2014) – Low Back Pain Tied to Spinal Endometriosis
Neurosurgery (Abstract, Aug. 2006) – Intramedullary Endometriosis of the Conus Medullaris: A Case Report
Climacteric (Abstract, 2008) – Endometriosis in PostMenopausal Women Without Previous Hormonal Therapy: A Report of Three Cases
Word Journal of Oncology (see Table 1 for a breakdown of those seven case studies)
~ Again, I am a layman. I do not hold any college degrees, nor mastery of knowledge. Please take what I say with a grain of salt. If curious, do your own research 😉 Validate my writings. Or challenge them. And ALWAYS feel free to consult with your physician. Always. Yours ~ Lisa


I have stage two spinal endometreosis it first started in my pelvis to spine . I’m still under going all kinds of “lab rat” tests but the pain is like no other I’d give child birth with no meds a 3 out of 10 in comparison.
LikeLike
I am so sorry to hear that, Summer. Continue to be strong
LikeLike
Thank you I will 😉
LikeLike
Is it possible to have your back pain be the primary symptom? Both my daughter and sister have had surgery that confirmed endometriosis. I have always felt I lucked up in not having that. They have severe pelvic pain which I don’t, (just normal achy throbbing for a couple days) however I have had severe back issues (the only one in my family) since I was 29/30, I am now 44 and just recently got seen by a back doc who said that it looks like just normal aging degenerative disc issues from an x ray – no mri. I’m not sure why I would have had that at 30, but didn’t think to ask that – just took the info as an answer. The physical therapist he sent me to said that the severe pain I have every time I sneeze (I have to brace myself or the pain will drop me) sounds like more than disc degeneration because the nerves have to be involved for sneezing pain like that. Anyway, my little sister was very sick this year and had to have surgery. They found endometriosis all over her intestines which was causing her problems keeping food down. I didn’t even know it was possible to have it outside of your reproductive system, and I started doing research because I have had significant digestive IBS since I was 15 and the idea that endometriosis could affect your intestines was new. I had never heard that in all the tests I went through growing up. While researching recently., I saw that severe back pain can also be a symptom too, so I began to wonder. I am just trying to understand why my back issues(the intestines I have just had to manage since high school) are getting so much worse and are now fictionally debilitating at times making me feel like an old lady already. I would’t even have considered endometriosis as a
possible cause if both my sister and daughter didn’t have it – and I didn’t just learn it can present differently than just severe pelvic pain. I just wanted to hear from someone who has this on their back/spine to see if I’m just grasping at straws for answers.
LikeLike
How could you tell you have it? I have stage 4 endometriosis and adenomyosis and I think I might have it in my spine. At times when I move certain ways it feels like I can’t move and my back hurts all the time. How did you go about getting diagnosed?
LikeLike
I am very curious how you got it diagnosed all my doctors say it’s not possible. I need to find out if I have it but not sure who to go to…
LikeLike
Please email or add me if needed
LikeLike
Hey Summer,
Wondering if I could contact you privately and ask you a few questions? My aunt had terrible Endometriosis, and also had it in her spinal region. It was so bad that she had a total hysterectomy at age 24. She never had kids. Anyhow, I’m following in her footsteps and have already had two surgeries for Endometriosis. I’m having horrible pain and am currently searching for a new gyno (I’m in Michigan). I can’t seem to contact you via this website, would you mind sending me an email if you see this post? Thanks!
petiteanomaly (at) yahoo (dot) com
LikeLike
How did you get diagnosed with spinal endometriosis? I often wonder if I have it as well.
LikeLike
I had surgery a year ago and have stage 3 endo. I have had severe back and sciatic pain go two years. My endo was on my bladder uterus and intestines. I asked my doctor about it and he told me to try fibrovan which is an herbal supplement that suppresses endometriosis and he said if my pain goes away from taking it… It’s most likely the cause. I also have polycystic ovarian syndrome and hashimoto’s hypothyroidism, I just recently started thyroid medications since hashimoto’s can also cause joint pain I want to see if my symptoms improve with that alone first
LikeLike
Good luck and keep us posted!
LikeLike
i also have Hashimotos, and Lupus, Endometriosis of course… adrenal insufficiency. i am a mess and only 32 years old feeling 90. i am unable to work but not deemed disabled enough to get SSD. i feel stuck. doctors dont understand. i am on cymbalta, hydrocortisone (cortef), nature throid very small amount, gabapentin which makes me even more of a zombie… sigh… i am at the end of my rope here. have no life. stuck in bed. waiting to die i ferl, this is not how life should be lived.
LikeLike
I, too, would like to know how your spinal endometriosis was diagnosed. I have had one area on my back/spine that used to flare up the first 2 days of my period and cause extreme pain, nausea and diarrhea. Now that I have had a total hysterectomy and oophorectomy, I continue to have pain in that same are. My MRI just showed a bulging disc at T7/T8 but I’m wondering if that could have been misinterpreted and might, in fact, be endometriosis. What type of doctor do you see that is so forward thinking? Every doctor I’ve talked to about this immediately dismisses endometriosis on the spine. I’d really appreciate any feedback!
LikeLike
Almost 2 years of back pain and sciatica getting worse with each period and worst of all with middleschmertz on right side. 2x ultrasound tech has said my right ovary looks funky and even said she could tell a cyst burst and fluid was in my pelvic cavity. Gyn says it’s all totally normal. I just had an MRI of my spine but it was 2 days past the horrible ovarian pain so I’m anticipating it all looking fine to my male osteo. How the poo do you get a Dr to consider it?
LikeLike
Have you looked at Nancys Nook on Facebook? There you will find lists of specialist surgeons all over the world that treat rare forms of endometriosis. Nancys Nook is an excellent resource to educate yourself on what endometriosis is and isn’t. She is a retired RN nurse that worked alongside Dr. Redwine. Please look her up and you will be glad you did. I am the information I have found has saved my life.
LikeLiked by 1 person
Yep, I’m a member of the Nook 🙂
LikeLike
I had an MRI done for back pain two years ago and in it it showed I had a hemangioma in L1 vertebral body.. I am currently following with a gynaecologist and have an endometrium cyst in my ovary and have all signs of endometriosis.. including very bad back pain.. could this be spinal endo?
LikeLike
All I keep hearing is how incredibly rare it is to have Spinal Endo, but I will never, ever, ever tell you it can’t be. 😉 Have a nice long discussion with your gyno. Bring studies if you need to (check out the links in my blog resources). And get referrals to the appropriate physicians who may help you determine that. It’s all about self-advocacy and pushing for answers. ❤ And keep us posted!!!!
LikeLike
i also have Hashimotos, and Lupus, Endometriosis of course… adrenal insufficiency. i am a mess and only 32 years old feeling 90. i am unable to work but not deemed disabled enough to get SSD. i feel stuck. doctors dont understand. i am on cymbalta, hydrocortisone (cortef), nature throid very small amount, gabapentin which makes me even more of a zombie… sigh… i am at the end of my rope here. have no life. stuck in bed. waiting to die i ferl, this is not how life should be lived.
LikeLike
oh man, Ashley. I am so sorry and wish I had some encouraging words to offer you that you haven’t already heard, and very likely rolled your eyes at ❤ Are you able to appeal the SSD decisions and keep pushing? I have a friend whom it took four appeals until she finally received her SSD.
LikeLike
Thank you thank you thank you for sharing your story! I have had symptoms of ms had an lp done and was told I have a lot of these bands that they check for but it was in my spinal fluid and cerebral fluid but they couldn’t figure out why I have told every doctor about how I have endometriosis and my symptoms are horrible during ovulation and menstruation. I asked about if and they said no that had nothing to do with endometriosis you can’t get it there. I can’t tell u how many doctors I’ve been to and how many look at me like I need to be committed. Thank u so much and if you wouldn’t mind messaging me or reaching out I really would like to talk with someone. Xox wishing you health and wellness always
LikeLiked by 1 person
Brittany, feel free to print out the studies linked in the Resources section and bring them to your doctors 😉 It’s what I would do if I had suspected it on my spine. ❤
LikeLike
Thank you so much for posting this info and the links. I have stage 4 Endo, diagnosed 5 years ago, with one ovary removed because I had an endometrioma large enough that caused the ovary to twist. None of my other endometriosis was removed during that surgery because it took so long to separate this from my bladder, ureter, colon, etc. I have had progesterone for the last year and a half because the pain that had been relieved came back, along with worse IBS pain. About a month ago I started having severe pain in the tailbone/sacral area, seeming to be worse when the Endo flares up. I really didn’t expect to find anything when I looked for spinal Endo, I thought maybe I was attributing normal aches & pains of aging to Endo, but it seemed a really strange place to have back pain because it’s lower than the lumbar part of the spine, which is the common place for back pain. Your info has helped light a fire under me to do more research and get some answers!
LikeLiked by 1 person
You are so welcome!!! Although I’ve read the spinal endometriosis may be incredibly rare, it’s worth a conversation with your doctor. Also, I have severe tailbone/lower back pain as a telltale sign that my Endometriosis is returning – and I don’t have it on my spine. I do; however, have a history of having it in my Pouch of Douglas (aka the cul-de-sac) – it’s the void between your rectum and your uterus. In both of my surgeries, it was noted my cul-de-sac was “obliterated” with Endometriosis…and after both of the surgeries (my Endometriosis was excised in both), my back pain disappeared. It was incredible. Barely there on my periods, even. I blame the lesions so near to my lower back inflaming and causing that lower back pain and aches. Since your Endo wasn’t removed, you too may have Endo affecting your Pouch of Douglas…or adhesions (scar tissue) may be wreaking havoc. Or it could be a whole slew of other reasons. I am so sorry that your doctor was unable to remove your Endo. Any thoughts on going in for another surgery to focus on removing the rest of it? Google “Where is the Pouch of Douglas” and find a photo of the side view – it will show the uterus, the rectum…and that very low point on your back – I’m curious to know if it’s similar to where your pain is. Again, though, arm yourself with research and go to your doctor. And no matter what, please pursue an excision surgery to clear out what’s still in ya. It may make a big difference. ❤ And keep me posted, woman! Now you're stuck with me. xoxo ~Lisa
LikeLike
I have Endo on my pouch of Douglas. Also on my uterosacral ligament which is attached to the sacrum (tailbone) lower pelvic spine. I suspect it in my lumbar spine (L4/5 area) as I have bulging discs and a radial tear.
I have read that having Endo in the Pouch of Douglas immediately qualifies as stage 4 based on position. Once it’s buried in far enough there is no reaching it beyond the ‘pouch’ – it is referred to as deep infiltrated Endo.
I suspect it is in/on my lungs.
LikeLike
I am a mother of a 15 year old daughter who may have spinal endometriosis. She has had constant back pain for over 8 months, had endometriosis diagnosed and removed in her uterus a month ago, but still has continued back pain. We saw several different kinds of doctors and 4 gynecologists before we came across one who took us seriously and would do surgery to look for and remove endo. Tricky when you are so young. May go back to orthopedic surgeon who couldn’t find anything from MRIs. Not sure if endo specialist would be more helpful though or orthopedic surgeon? Will do more research. Thank you for all this information.
LikeLiked by 1 person
I was diagnosed when I was 18. I was my gyno first patient with it. So he had to do a lot of research as did I. I had to have a radical hysterectomy at the age of 21 the lesions caused everything to ball up and made it impossible for me to have children. I am 31 now and I have always suffered from back pain but now it is so bad that nothing is really helping. They said I have disgenitive disk disease but only in one spot. I see pain mgmt chiropractor and do physical therapy. But it just makes it worse. I was googling to see if it is even possible and now I know. I know i still have it when i had my gallbladder taken out the dr looked and told me it was still there. I am on 2mg of estrace and they will not go up bc of it. This is something that we should have been told. To me this is s like cancer it spreads everywhere. Thank you for your blog and what everyone has commented bc now I think this should be looked into before I let them stick a needle in my spine to numb the pain.
LikeLike
I came across this site only today. I was looking up causes of chronic and unrelenting back pain, plus spinal damage. Now – I am reading this with no sense of surprise whatsoever, other than surprise that I have not been told I have spinal Endometriosis.
I live in the UK, and was diagnosed several years ago with Endometriosis. I had symptoms as a teen (painful, heavy and irregular periods) but these were just dismissed. I had symptoms again from 2002 (in my 30s) and finally had a lap surgery in 2011. Yes! It too TAT LONG! The NHS is utterly crap at treating Endometriosis. Doctors here in the UK are utterly rubbish at spotting the disease. For years, I was told different things. I was told I had irritable bowel. I was told it was “stress”. I was told it was just “normal period pain”. I was told my symptoms were “in my head”. The way the NHS treats people who have Endometriosis is utterly insensitive, uncaring and disgusting. You are made to feel like a Hypochondriac, which is so not true.
I had lived with back pain, hip pain on the left side, pelvic pain, anaemia due to heavy periods, bloating, cramping, upset stomach, nausea and vomiting – all which were worst during my periods – since early in 2000. I first started reporting these things to my GP in 2002. REGULARLY. I had to keep going back to the doctor over, and over again. Their lack of understanding, and complete inability to work out what was wrong, leaves me aghast! To this day, I cannot get my head around why it took my GP until 2006 to refer me to a GYNAE!
I did not get the correct treatment until 2011 when I had my first lap surgery. This was in BLACKPOOL (so anybody reading this who is treated there – BEWARE and move somewhere else because BLACKPOOL are TOTALLY INCOMPETENT). During this, they found Endometriosis and also claimed to have “removed it all”. They did NOT tell me where the Endo was, or how bad it was. They also DISCHARGED me the DAY OF THE SURGERY even though I was puking my guts up. Less than a week after the surgery I ended up in A&E because of extreme agony in my lower back, and inability to bend, stretch, straighten myself up, or turn. I was finding it hard even to walk. I got told the issue was muscular”. I was given ORAL MORPHINE. This occurred a further two times, and on one occasion I ended up in Hospital and was discharged only after seeing a Physiotherapist.
I continued in pain after the surgery, and was finally referred to an Endometriosis specialist (BLACKPOOL were NEVER specialists in Endo, so they by law, should NOT have done my surgery). I ended up having a further FIVE surgeries, including RADICAL EXCISION of deep infiltrating Endometriosis nodules from my left utero-sacral ligament. My specialist told me that the surgery done in Blackpool had a)missed these nodules, b)buried them under a load of scarring, and c)caused adhesions. I did get a bit of relief from further surgeries, but even after the radical excision, my symptoms slowly returned.
It is now three years since my last surgery. I have been told by surgeons that they do not wish to risk further surgery due to risk of damage. I had an MRI scan in 2015 that showed damage and compression to discs in my lower spine, and damage to my left sacro-iliac joint. This damage was passed off as “age related wear and tear”. I do NOT think this is true, because I have only had these problems since having Endometriosis and surgery. Besides, I am only in my 40s, so I struggle to see how I could have such extensive spinal and hip joint damage. Also, the hip joint damage is ONLY ON THE SIDE WHERE I HAD ENDO SURGERY.
I still have very heavy periods, bad enough to cause anaemia. I still have bowel and stomach cramping during my periods. I still have frontal pelvic pain. I still have lower back pain. I still have pain that makes me feel I need to pee lots. I still find smear tests agonising. I HAD ALL THESE SYMPTOMS WHEN FIRST DIAGNOSED WITH ENDOMETRIOSIS. I also have pins and needles in my left hip and leg when sitting. If walking long distances I get agonising hip and back pain. If I press hard on my lower back, right on where my spine is, these symptoms ease. I cannot lie on my front, because I cannot get up from this position – the pain it causes in my back and spine if I try to is agony.
So, I firmly believe I have spinal Endometriosis. The signs all seem to be there. I have even seen Physiotherapists, who offered STEROID INJECTIONS IN MY LOWER SPINE. Why offer this, if they do not accept there is a problem? The impression I am getting is that they KNOW THERE IS A PROBLEM, but are UNCERTAIN WHAT IS CAUSING IT.
LikeLike
Oh my god, Ella. First of all, thank you so much for sharing! Secondly, I am So sorry! I’ve heard that healthcare in the UK can be hard to get proper care for Endo…and it sounds like you’ve been through the gambit!!! UGH! Have you asked (or heard) about pelvic floor therapy? A few girls I know have received it (it can be painful) but it helps loosen up the muscles and nerves that may be in a constant state of flight or fright and causing major issues throughout. It may relieve some of your issues…maybe… I am so sorry I don’t have greater words of encouragment. 😦 Hang in there and continue to push, push, PUUUUSSSH. ❤
LikeLike
Wow sounds just like myself. I have it on my left uterosacral ligament and pouch of Douglas, I have scar tissue and nerve damage, constant back pain and sciatica, pins and needles etc. I have bulging discs and a radial tear in my lumbar spine and think it has travelled there. The uterosacral ligament is attached to the sacrum (tailbone in the pelvic spine) it makes complete sense seeing as well they’re connected that it would be in the spine itself. I cannot walk well anyway and live in constant pain however when I am due on and on my period I am beside myself with pain, I can only sleep on my right side with my knees together, semi fetal, so uncomfortable, huge amount of pain when resting, standing and walking. I find short relief on my knees leaning over something, constantly adjusting position, going out of my mind with pain. Ffs it’s in my right leg now, I’m in hell. So now my right arm is getting f’d up compensating for it. Also need to pee all the time, you may have a tilted uterus, as I have, normally the case in pelvic ligament damage apparently, ps all this I’ve researched because NHS are basically an emergency service now, unless you’re dying you’re not being treated. Referrals are like blood from a stone. Also was told for years that Endo wouldn’t affect your hip and leg, until I worked in obs and gynae and asked a consultant if it was possible, as soon as she said yes I went back to gp and got a referral, always suffered since day 1, I turned into a different person through puberty.
LikeLike