Here I go again, once more intrigued by Endometriosis growing in odd places inside the body. Today I’m going to focus on the appendix. I’ve read that many Warriors have their appendix removed because physicians may confuse Endometriosis pain for the symptoms of appendicitis. But on Tuesday an article hit my email about Endometriosis growing on the appendix…and I became obsessed.
Please remember: I don’t write this to scare you, or freak you out, or say that all of your right-sided abdominal pain is from Appendix Endo. Take a deep breath – I like to document these things in case anyone would like to discuss it further with their healthcare providers so they may be aware during surgery. Appendiceal Endometriosis is considered extremely rare and it is suspected that only 1-3% of all cases of Endometriosis involve the appendix. But…knowledge is power.
In November of 2018, I underwent my fourth Endometriosis-related surgery and am my very own walking case of appendiceal Endometriosis!
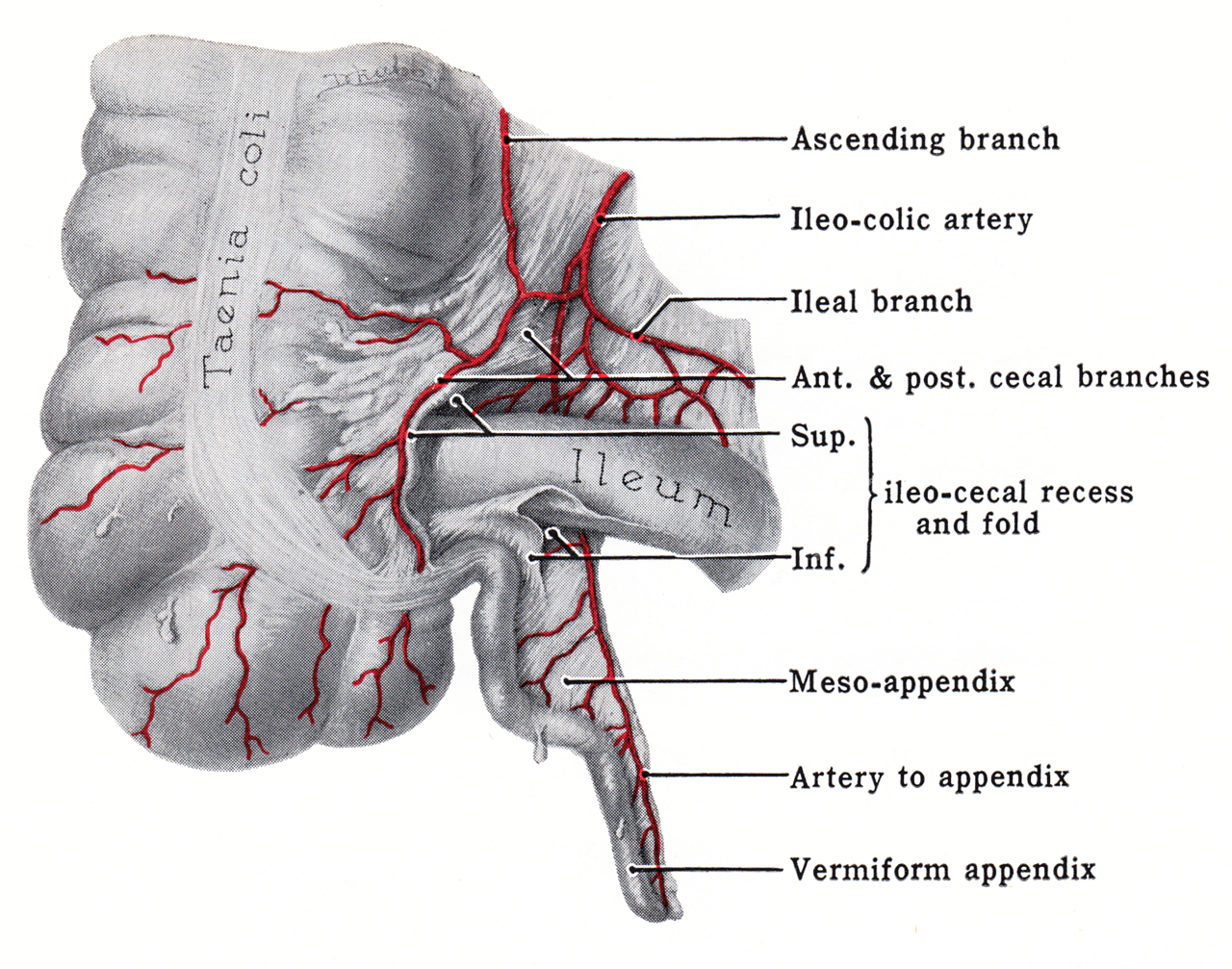
What & Where is the Appendix
The appendix is part of the gastrointestinal tract attached to a section of the large intestine, where it meets the small intestine. It is located in the lower right section of your abdomen, and is a skinny 4″ long tube. If you have pain in that location, especially when it’s pushed on, physicians may suspect appendicitis.
Appendix: Necessary Organ or Leftover, Useless Tissue?
Depending on who you ask, the appendix does (or doesn’t) serve a purpose. Hence why so many people no longer have theirs. If it’s inflamed, it’s typically removed.
Many believe the appendix to be a “vestigal organ” or an organ that used to have a purpose, but has since evolved into uselessness. Recently, though, some researchers have theorized that the appendix is not a useless flappy tube, rather it houses good gut bacteria – aiding in recovery from GI issues and illnesses and strengthening the immune system.
Is it useless? Does it safely store good gut bacteria? Who really knows…
Endometriosis versus Appendicitis
Symptoms of appendicitis can include fever, abdominal pain, abdominal swelling, loss of appetite, vomiting, an inability to fart (yes, I said “fart”), constipation, or diarrhea. Many of these symptoms can mirror complaints and symptoms of Endometriosis. Hence, an often misdiagnosis of appendicitis.
Appendicitis may develop because of inflammation, an infection, or even a blockage to the appendix. When infected or blocked-up, the bacteria inside the appendix goes nuts, the appendix can fill with puss and swell up. If left untreated, it can burst or rupture…which simply means it tears. It shouldn’t pop like a balloon. If it does rupture,the nastiness-fluid from within can spread all over the pelvic cavity, which may infect other organs or even cause sepsis, which can be fatal.
Is every bit of lower right-abdominal pain associated with appendicitis? No. It could just be something you ate, bad gas, period cramps, anyyyything. Or it could be appendicitis. AND some patients with Endometriosis of the appendix don’t have any symptoms – it’s just discovered by accident.
But that being said: sometimes Endometriosis can affect the appendix…One study stated that out of 1,500 appendectomy biopsies, 0.80% had Endometriosis. I’ve read that some surgeons believe that the appendix should be removed during Endometriosis excision surgery as a preventative measure, even if it appears healthy.
If you’re worried, please do your research and talk to your healthcare provider. As usual, there doesn’t appear to be any type of pre-operative diagnostic tests for the presence of Endo on the appendix. Ya gotta go in and see it for yourself…aka surgery.
Now, for the SCIENCE!
Documented Cases of Endometriosis on the Appendix
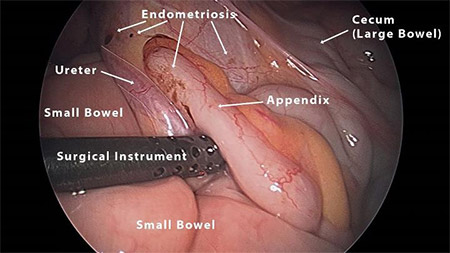
And before you bury yourself in reading numerous cases of patients with Endometriosis of the appendix, I wanted to share an image with you of what Endometriosis on the appendix can look like. Dr. Andrew S. Cook of Vital Health took this photograph during an excision surgery and has granted me permission to share it with you today:
Endometriosis on the appendix is nothing new – as my research will show.
The earliest published study I found online featuring Endometriosis on the appendix was published in 1929 in the Canadian Association Medical Journal. It covered three cases of women with Endometriosis: one with an Endometrioma, the second with Endometriosis on her appendix, and the third with Endometriosis in a surgical scar. I find it incredibly interesting that they dissect the theories of Endometriosis for each: contributing the first to Sampson’s theory, the second they simply note as “an unusual situation”, and the third they cite the German’s theory of tissue change (metaplasia). Just a fun little piece of historical literature on our disease. (I sense a new obsession festering…)
In 1960, medical records were reviewed from 30 appendectomies which occurred between 1919-1955 at St. Luke’s Hospital in Chicago, Illinois. Each was pathologically confirmed as Endometriosis of the appendix. Of those 30 women, 11 presented with symptoms which mimicked appendicitis. Four of those 11 presented with pain at the onset of their periods. It was noted that none of the 30 women had recurrent symptoms after their appendectomies, although many of them were found to have pelvic Endometriosis. Sixteen of the 30 women also went through partial or full hysterectomies at the time of their appendectomies.
In 1975, researchers combed through medical records of the Kapiolani Hospital in Hawaii and reviewed 12 documented cases of appendiceal Endometriosis, ranging from 1968-1973. During those years, the Hospital performed 1,496 appendectomies – of those, 12 tested positive for Endometriosis of the appendix. Additionally, the researchers interviewed the 12 women for further details and information. Many were found to have Endometriomas during surgery, too. Seventy-five percent of those women complained of abdominal pain prior to their surgeries. Which means, some didn’t – they had complaints of lower back pain and period pain. Unfortunately, the study doesn’t go into detail of how they fared after their surgeries.
A study published in 1981 documents a 23-year-old Nigerian woman who was 35-weeks pregnant and had complaints of vaginal bleeding and right-sided pain. Appendicitis was suspected, so a surgery was performed and her appendix was inflamed and torn. Her appendix was removed and the child was safely delivered by c-section. A biopsy revealed Endometriosis along the appendix wall where the rupture occurred, but nowhere else.
Another study in 1981 reviewed the medical records of 50 patients diagnosed with Endometriosis between 1968-1978 at Mount Carmel Mercy Hospital in Detroit, Michigan. Of those 50, 16 had confirmed Endometriosis of their appendix, the youngest of whom was only 14 years old…and the oldest? Sixty-two! Their complaints ranged from abdominal pain, to heavy periods, to GI complaints. Many had pain located in their lower-right abdominal quadrant. Pre-operative diagnoses included acute appendicitis, uterine fibroids, and ovarian cysts. During surgery, two were found to have ruptured appendixes with abnormalities, six had inflamed appendixes, and eight had normal-appearing appendixes. Seven of the 16 women also had total hysterectomies performed at the time of surgery. Biopsies on all confirmed Endometriosis. After surgery, two had recurrences of Endometriosis and it was later discovered in their sigmoid colons.
In 1983, a study reviewed the literature and medical records from 1950-1981 from the Department of Pathology Frederiksberg Hospital in Denmark. During that time period 10,000 appendices were removed and biopsied. Of those, 22 tested positive for Endometriosis of the appendix. Of all of the medical records reviewed during that time period, 800 patients were found to have Endometriosis.
In 2007, a study was published about a 35-year-old Japanese woman who complained of three days straight of abdominal pain (especially on the right side) and nausea. She had a history of mildly-painful periods, and had finished her last one three weeks prior. She was admitted into the hospital and imaging studies revealed fluid within her pelvic cavity, as well as inflammation of her pelvic lining. The physicians suspected either a perforated/ruptured appendix or a ruptured ovarian tumor or dermoid cyst. Surgery was performed and the appendix was found to stuck to her abdominal wall and was also “markedly enlarged” – so it was removed. Biopsies confirmed the appendix wall had been infiltrated with Endometriosis and likely caused her appendix to rupture. She was discharged two weeks later and was doing well.
In 2008, a study was published about two women in Turkey with appendiceal endometriosis. A 45-year-old woman went to the ER because of severe pain and nausea during the second day of her period. Lab work and imaging studies revealed nothing out of the ordinary, but she was tender to the touch. Due to the progressive severity of her pain while at the hospital, a laparotomy was performed and her inflamed appendix was removed. The interior wall of her appendix was confirmed by biopsy to to have Endometriosis present. Secondly, a 41-year-old woman went to the ER because of nausea, painful urination, and severe pain on the right side of her abdomen. Again, testing appeared mostly normal and due to the progression of her pain, surgery was performed. Her appendix was “covered with a brown-dark red colored material.” A ruptured endometrioma on her right ovary was suspected as having released the fluids throughout. Biopsy results yielded Endometriosis.
In Africa, a 2008 study was about a 25-year-old woman checked into the hospital with complaints of right-sided abdominal pain for the past day. She was also nauseous and vomiting. Lab results were normal and she was sent home and told to consult with a gynecologist. Three months later, she again went to the hospital with identical symptoms. The lab results were normal, but she was admitted for two days, then released. Four months later, she returned. This time she had the abdominal pain with diarrhea, but no nausea or vomiting. Tests showed she had a small cyst, and she was admitted for five days. Upon release, she was urged to consult with a gynecologist and a psychiatrist (I wish you could sense my anger as I typed that last word…). Nine months later, she was readmitted to the hospital for the same issues. This time, they performed an appendectomy and her appendix appeared normal…that is, until biopsy (yes, you guessed it) – it confirmed the presence of Endometriosis on her appendix.
In 2010, a study was published about a 29-year-old Japanese woman who had right lower abdominal pain for two days. She had similar symptoms about a year prior. She had a history of painful periods, accompanied by fever, and had been treating with her gynecologist with traditional Chinese medicines. Imaging studies showed a slight calcification and thickening of her appendix wall and she was diagnosed with acute appendicitis, and sent off for am immediate appendectomy. It was removed, appeared mildly inflamed, and was sent off for biopsy. You guessed it: Endometriosis. After surgery, she had no residual pain or feverish periods.
A 2011 study was of a 36-year-old Greek woman who complained of abdominal pain, swelling, constipation, and an inability to flatulate (is that a better word than farting? I think not. I still giggle.) for the past three days. She had a history of using contraceptive pills and painful periods. Imaging studies revealed a large blockage in her intestine which they presumed to be a tumor. She underwent an laparotomy, and they discovered numerous adhesions, an inflamed appendix, and her bowel was incredibly swollen. They removed the adhesions and her appendix and resected a large portion of her bowel. Pathology reports confirmed Endometriosis on her colon and her appendix. She treated with Triptorelin (a GnRH agonist) for her Endometriosis and six months later she had to undergo a second surgery to restore her resected bowel. No Endometriosis lesions were found and she was doing well.
A South African study published in 2016 study discussed a 33-year-old woman who had been suffering with infertility, even after three IVF attempts. She complained of pain to the right side of her abdomen for the last four hours, and was nauseous. She was hot to the touch, and tender at the right side of her stomach. Her pregnancy test and urine tests were normal, but given her infertility a CT was performed, which revealed a mildly-enlarged appendix, and let her physicians to suspect the onset of appendicitis. Laparoscopy was performed to remove her appendix, which was was visually inflamed, and while inside they noticed a “reddish brown area” on her uterus, which was excised and biopsied. Endometriosis was confirmed on her uterus and her appendix biopsy came back negative for appendicitis. However, her meso-appendix (a flap of connective tissue between the appendix and the ileum) did come back as having Endometriosis on it.
A study published in a Canadian journal in 2016 was about a 34-year-old woman who went to the ER due to right-sided abdominal pain. For the past several months, the pain had returned during her period, which she also started the day before she was admitted. All of her tests came back normal (except for a cyst spotted on her ovary), and she was discharged home. Five days later, she returned due to worsening pain. Due to the suspicions of appendicitis, surgery was ordered. Her appendix was not inflamed, but did have what was suspected to be a tumor – so the appendix was removed and sent off for biopsy. The results came back that Endometriosis was on involved with the appendix and mesoappendix. After surgery, she did not have any recurrence of pain.
Another 2016 study was of a 65-year-old woman in Turkey who had abdominal pain and nausea for the last 24 hours. She had pain on the right side of her abdomen and lab tests showed elevated inflammatory markers and enlarged appendix. An appendectomy was performed and a “brownish mass” was found on her appendix. A biopsy confirmed it was Endometriosis. She had no recurrent symptoms 30 months after her surgery.
In June 2017, the IJRCOG published a study from India of a 26-year-old woman with a history of Endometriosis. A year prior, she was diagnosed with an endometriotic cyst, and given six months of Lupron Depot, followed by a birth control pill, and was pain-free. Her pain returned chronically in her lower abdomen and she returned to her physician. She was one injected with Lupron Depot, but a week later her pain was so intense she went to the emergency room. Testing results raised suspicions of appendicitis. She underwent a laparoscopy, and she was found to have a dense adhesions, a frozen pelvis, and an inflamed appendix. Her appendix and adhesions were removed and upon biopsy her appendix was confirmed with Endometriosis. The authors conclude that appendix endometriosis is “very rare” and preoperative diagnosis is next to impossible.
In March of 2018, Obstetrics & Gynecology discussed the case of a woman with a known ectopic pregnancy. She also had a history of pain in her right abdomen. While they were inside her pelvis dealing with the ectopic pregnancy, they also performed an appendectomy based on their suspicions of appendicitis. Well, the biopsy results came back as positive for appendiceal endometriosis.
Another article published in 2018 was about a 42-year-old woman who presented with signs of appendicitis. A laparoscopic surgery was performed and a biopsy confirmed appendiceal endometriosis. A week after surgery, she had no recurring symptoms of pain.
An October 29, 2018, study found that a 40-year-old woman who complained of pain in the lower right of her torso ended up having Endometriosis on her appendix. She had a medical history of PCOS and uterine polyps. In addition to her right lower torso pain, she had lower back pain. Her pain had been going on for about two days. After a CT found a mass on her appendix, she underwent a laparoscopy and partial bowel resection. Four days later, she was released from the hospital. A follow-up MRI found that she had two Endometriomas on her right ovary. Now, what’s infuriating about that? Now she’ll need to go in for ANOTHER surgery to have those dealt with…*sigh*
On November 3, 2018, a study was published of a 29-year-old woman who started her period a day ago and then went to the Emergency Room because of radiating pain from her belly button down to her lower right quadrant. She was also nauseous and vomiting. Testing and palpitations were normal, the CT scan was unremarkable, but an ultrasound suggested she was suffering from appendicitis. A diagnostic surgery was performed and they found 30 ccs of blood (that’s a little over one ounce) in her pelvis due to a ruptured cyst on her ovary. Although the appendix seemed “contracted upon itself,” no traces of Endometriosis were visible. They removed her appendix and sent it off to pathology. Microscopic lesions of Endometriosis were, however, located on her appendix. Her symptoms stopped once she was recovered from surgery.
On November 26, 2018, I underwent my fourth Endometriosis surgery. Earlier in July, I went in for another excision surgery and it was discovered that I had Endo lesions on my small intestine, too deep to remove without a proper bowel resection. So, in November I went in for said resection. Not only was there endo on my small intestine, but also on my cecum, large intestine, and appendix. If you haven’t already read about it, feel free to explore my fourth Endo surgery!
A January 2019 study was of a 41-year-old woman who went to the ER due to lower right quadrant pain. A CT scan led doctors to suspect she had mucocele of the appendix: a blockage which led to a fluid buildup and secretion. She was given antibiotics, but two months later with ongoing complaints she underwent a surgery. The mucocele fluid had leaked from the appendix and invaded the sigmoid colon. The lesion had adhered her appendix to her terminal ileum as well as her sigmoid colon, so they removed her appendix and resected her sigmoid colon. Biopsy of her appendix found the blockage to have been caused by an Endometrial lesion, which caused the leakage and damage to her sigmoid colon.
A March 2019 study followed a 53-year-old woman who was admitted to the hospital for having lower right abdominal pain for the past three days, abdominal bloating for a week, and nausea, vomiting, and fever. A physical examination showed tenderness in her right lower quadrant. Doctors performed a laparotomy to see what was going on and found “copious pus” in her peritoneal cavity. Her appendix was removed and her peritonieal cavity was, in essence, washed out and scrubbed clean of pus. The appendix appeared normal, but during biopsy it was found to be covered in microscopic Endometriosis. The authors warn that Endometriosis may mimic appendicitis.
In July 2019, a study was published of a 35-year-old woman who complaint of lower right abdomen and hip pain for the past year and her pain was not only present during her period. She had a history of infertility, but that was it. A physical exam and blood work were normal. An ultrasound found a lesion in the right ileac fossa and thickening of the ileao-cecal junction (the valve between the small and large intestine). A CT scan showed a large tube-like growth on her cecum and led physicians to believe she had an acute appendicitis. Imaging studies also found multiple cysts on her ovaries. She underwent a laparoscopic appendectomy. The appendix was removed and sent off to pathology and confirmed as appendix endometriosis. Three months after surgery, she remained symptom-free.
Another July 2019 study was of a 29-year-old virgin who went to the emergency room due to abdominal pain and vomiting. She had suffered with those symptoms for a day, but had the same symptoms six months prior. She had no history of prior surgeries or Endometriosis. A CT scan showed she suffered from a small bowel obstruction. They suspected the blockage was caused by scar tissue (aka a band adhesion). Surgery was performed and the appendix was found adhered to the area where the large and small intestine meet. They also found blood in her pelvic cavity. The appendix was removed and the adhesions were removed. Pathology confirmed she and Endometriosis on her appendix and she was referred to a gynecologist for further treatment.
A November 2019 study focused on a 33-year-old woman who went to the ER with complaints of severe right abdominal pain for three days, nausea, vomiting, and a fever. For the past two weeks, she had passed “loose, watery stool” at least four times a day. The right side of her abdomen was tender during examination. Three years prior, she had a cystectomy due to Endometriosis and had dealt with infertility issues. An ultrasound showed an endometrioma on her right ovary and a small mass on her appendix, possibly appendicitis. Surgically, her right cyst was removed, as was her appendix. Biopsy confirmed the appendix mass was Endometriosis. She complained of pelvic pain six weeks after, but was referred to her gynecologist for further care.
In June of 2020, The American Surgeon published a study of a 45-year-old woman who had right-sided abdominal pain. A CT scan showed a small lesion on either her cecum or appendix. A colonoscopy revealed a mass on the cecum that did not obstruct the flow of her bowels. Surgery was performed, and they found that her appendix was glued to the cecum, both of which were removed. Pathology showed Endometriosis of both her appendix and her cecum.
A 2020 article published in the Journal of Medical Case Reports of a 45-year-old woman who had complaints of pelvic pain, painful sex, and painful periods. She had a previous surgery for Endometriosis as well. Her physical examination was painful and imaging studies found deep-infiltrating Endometriosis on her rectum, an endometrioma on an ovary, and nothing on her appendix. She underwent a surgery and, lo and behold, they discovered deep Endo on her appendix. They excised all lesions they found throughout her pelvic cavity and removed her appendix. Pathology confirmed not only was it endometriosis, but she also had a carcinoma on her appendix. She refused any further bowel surgery and was symptom-free two years later.
An October 2020 study states that Endometriosis of the appendix affects 0.05-1.69% of Endometriosis patients. In September of 2019, a 32-year-old woman went to the emergency room because of abdominal pain for the past 24 hours, which started in the upper abdomen and migrated to her lower right hip area. She was nauseated, vomiting, and unable to hold any food down. Her medical history and symptom didn’t raise any red flags, so lab work and imaging studies were ordered. A CT scan showed that the appendix was dense and enlarged and they suspected an appendicitis. Surgery was performed and the appendix was removed. No lesions or abnormalities were found within her pelvic cavity. Physically, it looked like just a regular appendicitis. But when viewed under the microscope, the pathologist diagnosed her with appendiceal Endometriosis, which led to the appendicitis.
The Asian Journal of Case Reports in Surgery published a study on March 8, 2021, of a 22 year-old-woman who went to the hospital for 5 days of throbbing right-sided abdominal pain. She had no other symptoms and reported it felt tender during any palpitation. Physicians suspected appendicitis and a surgery was performed. They noticed during surgery that her appendix was, indeed, inflamed. Everything else appeared normal within her pelvic cavity. The pathologist discovered Endometriosis within the muscle walls of her appendix. The patient was later referred to her gynecologist for any needed ongoing treatment.
In July 2021, the Clinical Case Reports published a study of a 38-year-old female who had complaints of abdominal pain (quantified at a six out of 10 on the pain-scale), right-sided tenderness, and nausea. She had no prior surgeries. And an ultrasound found a appendix was “thickened.” A surgery was performed, and they found “blood-tinged fluid” in her pelvis, as well as uterine fibroids, and an inflamed appendix which also had some gray growths on it. They removed the appendix and biopsy confirmed it was covered in Endometriosis. She stayed in the hospital for two days. Three years later, she was still symptom-free.
There were many, many more studies I did not highlight here. So many!!!
Again, if you’re worried, talk to you doctor. Supposedly it’s very incredibly rare to have Endometriosis of the appendix, but it does happen.
(Updated September 27, 2021)
Resources:
Acta Pathologica Microbiologica Et Immunologica Scandinavica (Abstract, July 1983) – Endometriosis of the Veriform Appendix
African Health Sciences (Article, 2008) – Endometriosis of the Appendix
American Journal of Obstetrics & Gynecology (Abstract, 1975) Endometriosis of the Appendix
American Journal of Obstetrics & Gynecology (Abstract, 1960) Endometriosis of the Veriform Appendix
American Journal of Surgery (Abstract, Oct. 1981) Endometriosis of the Appendix Presenting as Acute Appendicitis
Archives of Gynecology and Obstetrics (Abstract, 2008) – Appendiceal Endometriosis: Two Case Reports
Archives of Medical Science Civilization Diseases – (Article, March 2018) Appendiceal Endometriosis: an Unusual Cause of Acute Appendicitis
Asian Journal of Case Reports in Medicine and Health – (Abstract, March 2019) Appendiceal Endometriosis: A Case Report
Asian Journal of Case Reports in Surgery – (Article, March 2021) A Rare Case of Endometriosis Presented as Acute Appendicitis
BMJ Case Reports – Abstract, July 2019) Endometriosis of the Appendix Causing Small Bowel Obstruction in a Virgin Abdomen
British Institute of Radiology – (Article, Oct. 2018) – A Rare Case of Right Lower Quadrant Pain
British Journal of Obstetrics and Gynaecology (Abstract, April 1981) – Perforation of the Appendix During Pregnancy: A Rare Complication of Endometriosis
Canadian Medical Association Journal (Article, Sept. 1929) – Three Cases of Endometriosis
Case Reports in Gastroenterology (Article, June 2007) – Endometriosis of the Appendix Resulting in Perforated Appendicitis
Clinical Case Reports (Article, July 2021) – A Case Report of Appendicular Endometriosis
Ecronicon – Endometriosis of Appendix: A Case Report and Review of Literature
Everyday Health – What is the Appendix?
Healthline – What Does the Appendix Do? Things to Know
Case Reports in Surgery – (Article, Oct. 2020) Acute Appendicitis Secondary to Appendiceal Endometriosis
Hiroshima Journal of Medical Sciences (Article, June 2010) A Case of Endometriosis of the Appendix
International Journal of Reproduction, Contraception, Obstetrics and Gynecology – (Article, June 2017) – Concurrent Ruptured Endometrioma with Appendiceal Endometriosis: A Case Report
International Journal of Colorectal Disease – (Abstract, Jan. 2019) – Appendiceal Endometriosis Invading the Sigmoid Colon: A Rare Entity (you may access the full article here)
International Journal of Surgery Case Reports – (Article, Nov. 2018) – Endometriosis of the Appendix Presenting as Acute Appendicitis with Unusual Appearance
International Journal of Surgery Case Reports – (Article, July 2019) – Appendicular Endometriosis: A Case Report and Review of Literature
Journal of Emergency Medicine Case Reports (Article, 2016) – Two Cases of Acute Abdominal Intestinal Endometriosis
Journal of Medical Case Reports (July 2011) Rectal Endometriosis Causing Colonic Obstruction and Concurrent Endometriosis of the Appendix: A Case Report
Journal of Medical Case Reports (2020) Neuroendocrine Appendiceal Tumor and Endometriosis of the Appendix: A Case Report
Journal of Obstetrics and Gynecology Canada (Abstract, Oct. 2016) Isolated Appendiceal Endometriosis
Mental Floss (Article, undated) Immunology Study Suggests the Appendix has a Use After All
Obstetrics & Gynecology (Abstract, March, 2018) Appendiceal Endometriosis and Ectopic Pregnancy Occurring Simultaneously
Science Alert (Article, Jan. 2017) Your Appendix Might Serve an Important Biological Function After All
Science Daily (Article, Jan. 2017) Appendix May Have Important Function, New Research Suggests
South African Journal of Obstetrics and Gynecology (Article, Sept. 2016) – Endometriosis of the Meso-Appendix Mimicking Appendicitis: A Case Report
The American Surgeon (Abstract, June 2020) – Appendiceal Endometriosis Presenting as Possible Cecal Mass
~ Again, I am a layman. I do not hold any college degrees, nor mastery of knowledge. Please take what I say with a grain of salt. If curious, do your own research Validate my writings. Or challenge them. And ALWAYS feel free to consult with your physician. Always. Yours ~ Lisa


I’m a personal fan of remove the appendix as a preventative procedure while your physician is in there for “spring cleaning”. I had a complete justo at 28 ( yer 2000) due to endo eating through my large intestines (pathology confirmed and documented). 5 years later my appendix burst, and yes worst case scenario I had sepsis with a following two more surgeries, eventually leaving me heal with an open wound from the inside out.
There simply are not enough studies with supporting data to dictate a standard procedure for preventative removal of an appendix, but I sure wish I had such an opportunity . The appendix rupture was terrible to the point of last rights given.
Also not to scare anyone, but there are medically documented cases of endometriosis both the outside of belly buttons as well as even a finger tip… both bleeding on a monthly cycle and all documented as Endometriosis. Simply do your research and make the best decision for you and for your future. If you do have endometriosis, I’m so very sorry to hear that and prayers that it is a mild case with minimal negative impacts to your body.
Best regards
D-
LikeLike
Hello, long lost friend!! Just my 2 cents here, but during one of my endo surgeries the surgeon removed my appendix “while she was in the neighborhood” (her words) because she said endo could possibly grow on it. I don’t remember if she actually found any on there or not. I never gave consent for her to remove my appendix in the first place and was a bit PO’ed about not having a say in it, but from your science above, I guess she knew what she was doing! I’ve not noticed any difference from not having an appendix. In fact, it’s just one less thing to worry about IMO.
I MISS YOU! Hope all is well and that you’re enjoying married life. ❤
LikeLiked by 1 person
*smoooooooooooooooosh* I’m well! Busy as all muckity-muck though with work and life and haven’t had a lot of spare time for research and blogging! I neeeeed to 🙂 How have YOU been?!? I’m all curious now and want to know the biopsy report of your appendix 😀
LikeLike
Wow, OK. I’m currently recovering from surgery for appendicitis… and when they opened me up, they found endometriosis was the cause. I had atypical symptoms for appendicitis – no fever. But it was during my period, which I explained was heavy and frequent these days and so they wanted to operate. It’s all been a shock but I’m so glad a found this article and can see I’m not alone.
LikeLike
Hello !
I am currently scheduled for surgery for my endometriosis . They are removing my left reproductive side and my appendix as they are both compromised. I did not know this was RARE !
LikeLike
I’m two weeks post surgery. During a colonoscopy, they found a mucousceal appendaceal. Because of risking leakage from the mucousceal, they had to wait until after surgery to do biopsy. Because it could be cancerous they also took part of my colon. It turned out to be endometriosis. Now I’m researching endometriosis. Can it be in your appendix and not in other female parts or does it spread from female part? Within the past 7 or so years I have had two vaginal sonograms, biopsies and DNCs for uterine polyps. Could they be missing endometriosis?
LikeLike
Good morning. As endometriosis is typically found outside of the uterus and bowels, I’d recommend seeking a surgeon knowledgeable in excising endometriosis and having an exploratory laparoscopy. If they find it, they can cut it out. Imaging studies don’t usually show endometriosis. But only if it’s something you’re comfortable doing. And only if it’s a knowlegable surgeon. I’ve heard horror stories of surgeons who confirm the presence of endo, not remove it, and tell the gal she needs tosee another surgeon to remove it. And avoid ablation of endometriosis…all bad.
LikeLike
I don’t think I had it on my appendix but I did get appendicitis exactly one month after my Endo surgery. It actually stuck to a lesion removal site and I couldn’t tell the healing pain from the appendix pain until it was about to burst. Luckily we caught it in time and the removed my appendix and were able to get the infected first surgery site resolved.
LikeLiked by 1 person
I’m so glad you were able to catch it in time!
LikeLike
3 days after getting off my period I went to the ER for a mild sharp pain. I was pretty confident in knowing it was my appendix. I wasn’t in sever pain, just a tad uncomfortable. After running test doctors confirmed I had an appendicitis. After surgery I was told I had endometriosis. I guess it explained why I the pain of an appendicitis didn’t affect me. I was dealing with endometriosis every month thinking the severe pain was normal.
LikeLike
This is highly topical as I lay awake recovering from my recent appendectomy. I have had severe pain from periods ever since I have 14 with vomiting, sweating, passing out and bowel problems (all the fun stuff). Diagnosed ten years later with endo and started treatment in the form of progesterone implant called implanon. Eventually periods stopped but bowel problems continued after my lap and excision. Went back to doctor and was put on FODMAP diet and told to exercise more. Saw a therapist, did pelvic therapy etc but things got so bad to the point where I couldn’t work full time anymore. I was referred for colonoscopy. Result: I was told I had IBS and to do the FODMAP diet and spend a fortune on a particular probiotic called infantisbifidus or something. I continued my descent into misery as I was still sick all the time. Was referred back to gyno. CT scan showed nothing unusual, ultrasound normal. Had another lap. More excision of endo but no active patches and a mirena was inserted for good measure. Gyno did notice that my appendix was stuck to my bowels and that I had quite a few adhesions in the right side. She cut the sucker free and that was that. Months later I was still in pain. I’d given up and accepted that this is how life would be forever more until one day I couldn’t get into my regular G.P. I saw a new GP that asked me why I was getting anti nausea medication and why I accepted such a shitty standard of life for myself. She called my gyno immediately and told her to see me that day. My gyno recommended I visit a pain clinic to help manage my chronic pain but she also threw the idea of seeing a general surgeon into the mix. She said she’d noticed the bowel adhesions on the right side and since that was the site of my pain (predominantly) it might be worth talking to someone about. Three weeks later I strolled into the surgeons office and he poked my abdomen and told me to cough then asked me what I was doing tomorrow. Before I could answer he said ‘getting your appendix out.’ They confirmed upon removal that it was inflamed and even though it had been set free a few months earlier it had done a bit of dancing and gotten itself twisted and stuck again. Which brings me to tonight. I’m on day five of recovery waiting for pathology results to determine what the cause of my inflamed appendix was. It was suggested that it could be endo given my history but also that it could be nothing…guess I’ll just have to wait and see to find out. P.s if there is a moral to this story it’s that you shouldn’t wait for a doctor to tell you being in pain all the time isn’t normal. Don’t accept it, keep trying and eventually someone will listen.
LikeLike
Oh man…please keep us posted when you get those biopsy results! I’m glad that they took out your angry appendix and hope that your recovery goes well. Heal up, woman. And thank you for sharing such an incredible PS. We all learn the hard way, it seems. ❤
LikeLike
This is so refreshing to hear I’m not the only one!! I’m scheduled for a diagnostic Lap on the 19th, hopefully they will take out my appendix! I’ve had 2 surgeries in the past to remove extensive adhesions and endo, and a hysterectomy last fall that confirmed adenomyosis as well!! I’ve had this RLQ pain since august, and relentless bowel issues that CT and colonoscopy all say everything is fine…So ready to get rid of this pain that no one thinks is there!!!
LikeLike
Good luck, Kate!!!!!! I’ll be going in on the 26th for my bowel resection! Heal well, hun! ❤
LikeLike
Super interesting – thank you for pulling all of this together! I’m laid up in bed recovering from an appendectomy 5 days ago. Leading up to it I’ve had two years of gastrointestinal issues – episodes of severe distress including vomiting, diarrhea, and bloody stool…basically what looked like severe food poisoning but happened 4-6 times a year. I finally had a colonoscopy done which showed mostly normal except for a section of my bowel that appeared to be being pushed in from the outside. So they ordered a CT scan and then a MRI which both showed a mass on my appendix and fluid over my liver. Since the radiology reports both pointed out the mass and mentioned the possibility of it being cancerous, the general surgeon recommended taking my appendix out laparoscopically. The pathology results showed endometriosis on it. So here I am. I’m five days post surgery and in increasing amounts of pain and wondering now if I’m going to have issues with endometriosis in the scar tissue that is forming inside. What’s interesting is I’ve been asking if my symptoms could be from endometriosis and all of the doctors have told me no – yet here we are! Listen to your guts (literally and figuratively!) ladies!
LikeLiked by 1 person
Oh my gosh…
Seven years (so far) of presenting in emergency rooms with the same freaking symptoms, and never, not once was it mentioned that maybe I had endo on my appendix.
I finally see a specialist next month, but gosh it’s nice to know that I’m not crazy
LikeLike
Good luck and please keep us posted!!
LikeLike
Hello i love your article and all your resources and research! I just had my 6th abdominal surgery, 2 being c-sections and the other 4 were laporoscopy for endometriosis. Last year the emergency surgeon at the hospital performed a lap sx and said “you’re a hot mess in there!” Bladder fused to uterus, uterus and ovary fused to left pelvic wall, and adhesions and endo everywhere. She didnt remove any endo and was afraud of damaging my uterus and bladder so didnt seperate them. She did cauterize veins that ruptured from a ruptured ovarian cyst that was bigger than my ovary. One week ago today, I had a lap sx with my OBGYN surgeon and he removed endometriosis, adhesions, and seperated my uterus from the pelvic wall. He also was afraid to seperate my bladder and uterus. He took pictures and gave them to me of my appendix which was covered in endometrial tissue/webbing and he left my appendix due to it appearing perfectly healthy and normal. It’s funny to me that this is so rare because ever since my first pregnancy which ended in a ruptured ectopic in my right fallopian tube, ive been nothing but one of the rare cases on things after. I could go on and explain them all but it would end up being a book! Lol (this basically already is 😉 )
Anyway, thank you for writing this. It really helped me understand what ive been going through. Every doctor thought it was appendicitis and I had to argue my case that it was endometriosis. And now i have information to take to my follow up apt in a week! Im going to keep reading your articles!
LikeLike
Good luck!!!! Self-advocate and kick some butt!! Let us know how it goes and if you need anything
LikeLike
I also had to have my appendix removed because of Endometriosis covering it. I’m glad you are shedding some light on this subject!
LikeLiked by 1 person
Add my name to the list of this “rare” condition. Had extreme cramps and an assortment of symptoms with my menses all my life causing me to stay home in fetal position for hours on end. No doctors ever took it seriously. Then, after a year plus of taking Tamoxifen for breast cancer at age 57, I mysteriously had a case of appendicitis and upon removing it the surgeon had to perform a colon resection since my appendix was so fused to my colon. He never asked about my history of endo and it was my sister who asked him later if the cause could be this.The surgeon looked at her dumbfounded, but she turned out to be correct. He thought it was just more cancer. Reality is that tamoxifen can exascerbate the endo, not to mention can cause endometrial cancer, which, surprise of surprises, I also was diagnosed with a year after the appendectomy. Moral of the story ladies is to be careful with Tamoxifen, and share your endo history with all medical professionals, especially male ones.
LikeLiked by 1 person
I had my appendix removed after months of lower right quadrant pain. Lo and behold, it was endometriosis. This was 4 years after a total hysterectomy. I’ve now been having upper left quadrant pain for several years. I bring up edno, then am told I’m constipated. I am certain that the endometriosis is on my pancreas. No one will listen. Very disheartening.
LikeLiked by 1 person
I’m glad you got the endo on the appendix diagnosis! and re: your pancreas – keep pushing. it’s not unheard of! If you haven’t already seen it, here’s my blog entry on the pancreas and Endometriosis. https://bloominuterus.com/2019/01/16/endometriosis-the-pancreas/ Feel free to print out the studies in the Resources section and fling them at your physicians. ❤
LikeLike
Hi, this has been an interesting read. I have had a left ovarian cyst since January. Scans showed it was 3 x 2 cm and gave me a lot of pain when exercising along with pain on my lower right side. I had a laparoscopy in Monday and they removed the cyst and ovary and also my appendix as there were 2 lesions which they reckoned were endometriosis. Am now having to wait for the results of testing. The doctors didn’t seem too concerned, Said results would be posted to me, but I can’t help worrying that it is more sinister as I thought endometriosis on appendix was very rare. The cyst has never got any bigger, the lesions on the appendix seemed quite small and my full blood count was normal, but am so scared the results come back that it is cancer.
LikeLiked by 1 person
I’ve heard it’s rare, too, but with so many women in my life that had it on their appendix (myself included) I thinks “rarely diagnosed” is more appropriate. When will you get your r sults? 2 weeks?
LikeLike
Thank you so much for this. I’ve been in crazy awful pain the last month or so. Lower right pain that takes my breath away. In fact sometimes I have to measure out my breathes because I can’t inhale deeply. Then I started having that same pain in my upper left side. A odd thing is the complete horizontal of belly button to the right is numb to the touch.
I had a laparoscopy in 2006 because of a huge cyst on my right ovary, then they found Endo everywhere! Growing up my spine and all crazy places. I desperately wish I could find the cause of this pain.
I wonder if severe dry mouth, racing heart and inability to take deep breathes is connected… anyways, thanks for this great post.
LikeLike
You’re so welcome! Continue to track your symptoms, try to identify any patterns or triggers, and talk to your doctors. ❤ I hate that you're a part of the EndoFamily, but am oh so grateful you're not alone. ❤ We're in this together!
LikeLike