Susie is 41-years-old and was just diagnosed with a surprise Endometrioma in a very surprising location. She lives in Austin, Texas and is coming to grips with her diagnosis, as well as searching for answers and support.
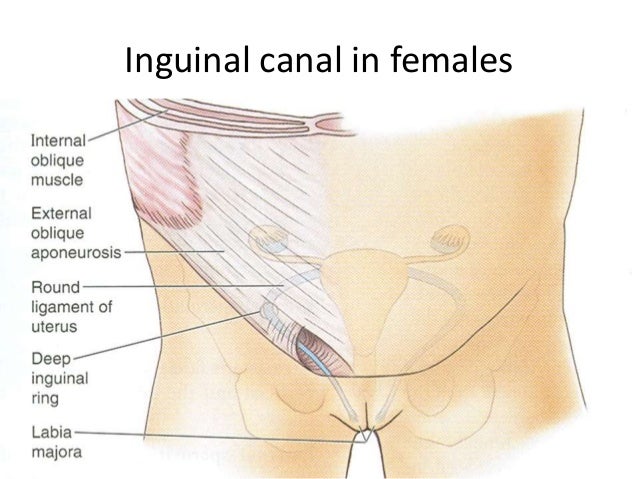
Susie’s Journey: I began experiencing symptoms of my disease when I was in my early 20’s around 2004-2006, I felt a lump on the right side of my groin that moved around a bit. I had a pap smear that showed normal results, then a sonogram that did show the mass, and then a CT scan that was inconclusive. I was told that cancer was ruled out and that they had no idea what it was, but that it wasn’t worth doing a biopsy over, but that if it ended up causing problems in the future, I might probably have to have one.
Being a young 20 year old, I feared the idea of anyone cutting my groin open and could not afford to get off of work for surgery anyway. I lived with the mass for over a decade. Throughout that time, I began noticing it growing larger and becoming more firm. It was no longer moveable and it swelled up around my menstrual cycle. The day before or the day I started my periods, there was extreme pain. The pain also continued up to a week after my periods. Sometimes, it made it a little difficult to walk and I’d get a bit of pain on my right leg, but not too much. It prevented me from moving and sitting freely. I couldn’t even cross my legs.
Fast forward to 41 years old, I finally decided that it was time to do something about it. I read up about endometriosis and even asked the doctor if it was a possibility. After about several pelvic exams, 2 or 3 sonograms, a CT scan, and a very painful biopsy that required 2 shots of local anesthesia in order to retrieve 2 samples of the mass, I was finally diagnosed with endometrioma.
I was given the option of excision or just living with it.
Doctor asked me if I’ve considered birth control and slightly suggested I use it. I told him that birth control would not remove the mass and did not help me much when I was on it in my 20’s and that I wanted this lump out of me. He said that he would perform a simple outpatient excision that would require very little (if any) time off of work and that I would be running around just fine afterwards. About 2 weeks ago, I finally had the surgery that did verify “endometriosis”. I was completely anaesthetized to sleep. Btw, I’m not sure what the difference of “endometrioma” and “endometriosis” is because both words keep getting used by my doctor and pathology report. My doctor corrects me when I call it “endometriosis” and says it is “endometrioma” and then the pathology report says “endometriosis”. My doctor seems impatient when I ask him to explain the difference. I almost wonder if he actually knows about what I have and doesn’t want to confirm my suspicion. I am in the dark about that right now.
WELL, I awoke from my surgery to find that my right foot and leg were asleep. I could barely move my toes. My feet have a tingly feeling and my leg has the same feeling as though it’s been asleep and is about to start waking up. I was told that because I could move my toe, it was a good sign and that I should be able to start walking just fine again in about a day. Since then, although, I regained some feeling back to the upper part of my leg and some of the left side of my right foot, I am experiencing Charley Horses” both in my sleep and mostly when I walk for the past week. I still have to walk very slowly with a cane and an extreme limp.
Yesterday, I was admitted into the emergency room to check for DVT (Deep Vein Thrombosis aka “blood clots in the leg”) but I checked out clean. The emergency staff told me that I did not suffer from dehydration and that my potassium levels were fine and that all he can think is that maybe my leg’s nerves are cramping because they are “waking back up”. I don’t know if I’ll be able to walk like normal again. It’s very hard for me to get around at work and college classes are difficult to get to. I have to have people do things for me. I had to cancel my birthday plans to go to the beach because I don’t think I’ll be able to walk around in the sand and the idea of a wheelchair is very depressing. I am getting married in October and am mortified of the idea of having to walk down the aisle or live my life with a cane. My follow-up appointment with my surgeon is next week. Although, I hope that I will be okay by then or that he’ll be able to help me, I don’t know if he’ll have any help to offer. It’s scary how little the medical industry knows about endometriosis. What is wrong with my leg???! Also, now I’m hearing that just because you have endometrioma excised doesn’t mean that it won’t come back and that I should consider a hysterectomy. I don’t want to go through this again. I almost regret having the surgery in the first place. I hope that it was worth it and that I will be able to walk again.
Words of Advice: Read as much as you can about it. Meet as many people as you can. Ask as many questions as you can. Don’t give up.
The Last Word: I hope that we can get more endometrioma awareness outreach out there.
If you would like to e-mail Susie, please feel free to.
I want to send a special Thank You out to Susie for being brave enough to share her journey with us today! Congratulations on your upcoming nuptials!! And good luck with your healing and the circumstance with your leg. You have my email address, woman – keep me posted!! ❤ Yours, Lisa.
And if YOU would like to share your story, send it to me; I’d love to share it. The best part about this disease is the strong network of love and support from our fellow EndoSisters, and our friends and family, too.