A new study about Endometriosis is out regarding the modern treatment of the disease. This includes birth control, progestins/anti-progestins, GnRH agonists, aromatase inhibitors, danazol, NSAIDs, surgery, and alternative treatments. It identifies the pros and cons of each.
The study closes with this beautiful phrase:
“The pharmaceutical or surgical treatment require an individual approach and deliberated informed consent of the patient. Pharmacological treatment is only symptomatic, not cytoreductive, therefore, to remove endometriosis lesions, surgery should be performed.”
It’s uplifting to see a study bluntly state that medications only treat the symptoms, NOT the disease itself, and the Endo lesions need to be removed. AND that each case of Endometriosis must be reviewed on an individual level.
“Deliberated informed consent of the patient” means (to me) as having a fully-informed patient who is made well-aware of the pros and cons of each choice, the side effects, risks, and potential outcomes; as well as having performed their own research before agreeing to the treatment.
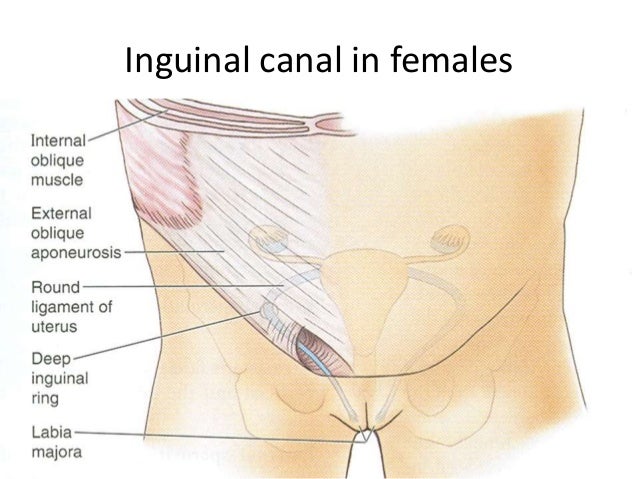
Even with excision, though, there’s always a possibly of recurrence or new growths. And not all physicians are skilled enough to recognize each lesion. Not to mention many surgeons still practice ablation (the burning away of the lesion, leaving rooted tissue to regrow).
Welcome to an EndoWarrior’s very frustrating pursuit for competent medical care.
I encourage you to read the study for yourself and share it.
Resources:
Journal of Education, Health, and Sport (Article, 2019) – Available Treatment Methods for Endometriosis